Introduction
Hemolysis is a well-recognized clinical observation in a subset of myelodysplastic syndromes (MDS) patients (pts). However, the clinical consequence of hemolysis and the associated molecular phenotype in MDS is not well described in the literature. Nonimmune hemolysis in MDS is often attributed to ineffective intramedullary erythropoiesis or acquired hemoglobinopathies that have been described in rare cases of MDS. In this study, we report the prevalence of hemolysis among MDS pts, their clinical and genomic characteristics and its impact on outcomes.
Methods
We identified all pts in our institutional MDS database who had serum haptoglobin measured at time of diagnosis or referral. We considered serum haptoglobin < 10 mg/dl as a surrogate marker for intravascular hemolysis. We compared the baseline characteristics, response to treatment, and overall survival (OS) in those with hemolysis (haptoglobin < 10 mg/dl) to those in the non-hemolysis group. Further, we explored the mutational landscape among pts with hemolysis compared to the non-hemolysis group.
Results
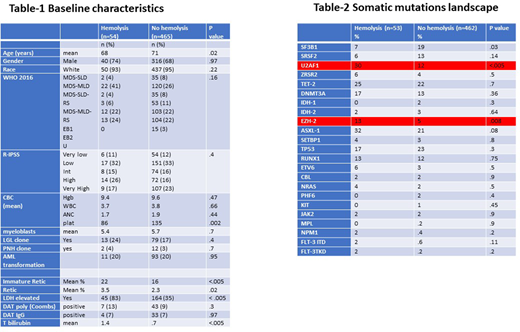
Among 519 pts in our database with a known serum haptoglobin at first referral or diagnosis, 54 pts (10%) had serum haptoglobin < 10 mg/dl (the hemolysis group). The baseline characteristics were similar among the two groups except for a slightly younger age and lower platelets count in the hemolysis group. Other laboratory markers associated with hemolysis such as total bilirubin and LDH were significantly increased in the hemolysis groups. However, no difference was seen in coombs test results. Only 13% versus 9% were Coombs positive suggesting that hemolysis in MDS is typically not immune mediated (table 1).
The median OS was 31 months versus 39 months among pts with hemolysis and no hemolysis respectively, (p=.98). There was a trend of inferior survival among pts with hemolysis in the low and intermediate risk revised IPSS (R-IPSS) risk groups. The median OS was 44 months with hemolysis compared to 89 months with no hemolysis in low risk R-IPSS (p=.2) and 19 months versus 34 months in intermediate risk group. (p=.7)
The hematological improvement (HI) rate using erythroid stimulating agents (ESA) was 16% (3/19 pts) in the hemolysis group compared to 30% (39/130 pts) in the non-hemolysis group. (p=.2) The HI+ best response with hypomethylating agent (HMA) was 70% (22/31) compared to 45% (127/280) among hemolysis and non-hemolysis groups respectively, (p=.05).
Table-2 summarizes the somatic mutations landscape between the hemolysis and non-hemolysis groups. U2AF1 and EZH2 hotspot mutations were statistically significantly more common among hemolysis group. Out of the 16 pts with U2AF1 mutations, 15 (94%) harbored a mutation at serine 34 (S34) in the hemolysis group while only 22 of 55 (40%) cases with U2AF1 mutation had an S34 hot spot mutation in the non-hemolysis group suggesting that the association between U2AF1 and hemolysis is allele specific. (p .0001)
Conclusion
Non immune hemolysis was observed in 10% of MDS patients. Inferior survival trends were observed among lower risk MDS patients with hemolysis. A decreased response rate to ESA and higher responses to HMA were also observed in the hemolysis group. U2AF1 mutation was observed in 30% of patients with hemolysis and occurred almost exclusively at the S34 hot spot. Our data suggest that nonimmune hemolysis is associated with allele specific somatic mutations and associated with key clinical outcomes. Future work will explore the contribution of altered splicing to these acquired hemoglobinopathies.
Komrokji:BMS: Honoraria, Speakers Bureau; Novartis: Honoraria; Incyte: Honoraria; JAZZ: Honoraria, Speakers Bureau; AbbVie: Honoraria; Agios: Honoraria, Speakers Bureau; Acceleron: Honoraria; Geron: Honoraria. Sallman:Celgene, Jazz Pharma: Research Funding; Agios, Bristol Myers Squibb, Celyad Oncology, Incyte, Intellia Therapeutics, Kite Pharma, Novartis, Syndax: Consultancy. Padron:Novartis: Honoraria; Incyte: Research Funding; Kura: Research Funding; BMS: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal